Ekene Onwuka, MD, grew up in Gary, Indiana, a small blue-collar town outside Chicago. Like many cities that relied on the steel industry, Gary had its share of economic struggle. So once Onwuka reached 10th grade, he seized the opportunity to attend an elite Massachusetts boarding school through a program called A Better Chance — in hopes that it would bring him closer to his dream of becoming a surgeon.
“Boarding school was the first time that I was introduced to the fact that maybe everywhere wasn’t like Gary, Indiana,” said Onwuka, who is now a pediatric surgeon with Texas Children’s Hospital in Houston. “It was just a completely different environment.”
Onwuka started to wonder how the stark differences between communities and economic circumstances could shape children’s lives, including their health. Eventually, that curiosity inspired him to pursue cancer disparities research. The need to expand disparities research hits home every time he meets a patient from an under-represented background, especially when a child is diagnosed with cancer at a later stage. “It’s always at the back of your mind,” he said. “There’s always that feeling of, ‘I wonder why this is?’ and a desire to dive into it a little bit more and try to figure it out.”
Now with support from Children’s Cancer Research Fund (CCRF), Onwuka is studying the connection between genetic ancestry and treatment outcomes in children with rhabdomyosarcoma (RMS), a cancer that affects the body’s soft tissues.
The role of genetic ancestry
Unlike some other childhood cancers, the outlook for RMS patients has not improved in recent years: five-year survival rates are less than 70% and fall to 30% for kids whose cancer has metastasized. African American children with RMS face a 16% worse survival rate than their non-Hispanic white peers. But Onwuka, who is one of the inaugural recipients of CCRF’s new Disparities Award, hopes that fresh insights into the role of genetic ancestry could hold the key to more effective treatments.
“Ultimately, it is our goal to help children diagnosed with RMS experience fewer side effects from their treatment and to live longer lives,” he said.
At-home DNA kits from companies like AncestryDNA and 23andMe have become popular ways for people to understand more about their family history, but genetic ancestry can also reveal important clues related to health risk. Ancestry data can also be more helpful and precise than when patients self-identify their race or ethnicity.
“Genetic ancestry testing is becoming important in medicine,” he said. “We now know that individuals descended from certain regions or groups have variations in their genes that can put them at risk for disease and impact their response to drugs. We believe this to be the case for children with RMS.”
While other studies have examined the role of genetic ancestry in blood cancers, such as acute lymphocytic leukemia (ALL), Onwuka is the first to explore genetic ancestry in RMS.
“The main goal is to try to figure out whether there are certain genetic predispositions that lead to poor outcomes in patients with rhabdomyosarcoma,” he said.
Understanding risk and how to improve outcomes
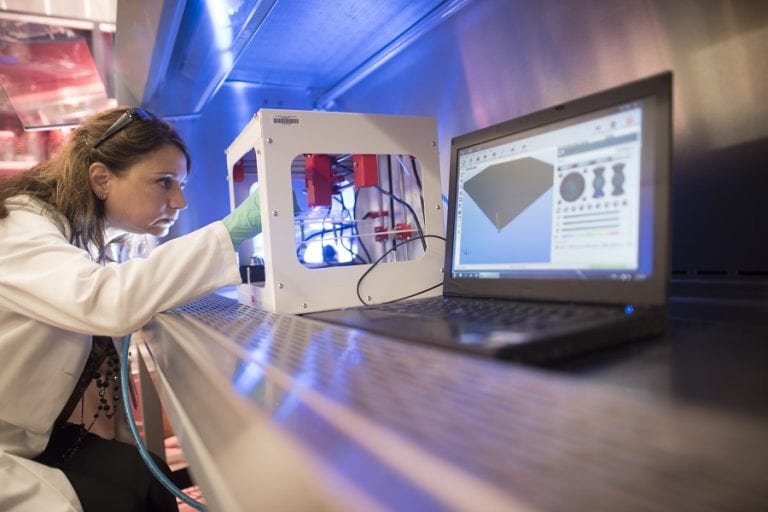
Onwuka is analyzing more than 900 samples from pediatric patients who participated in Children’s Oncology Group studies — one of the largest and most diverse data sets assembled on RMS patients. He will measure genetic ancestry in children to identify whether specific ancestries are associated with worse toxicities and survival rates.
If the data shows that genetic ancestry has a significant impact on outcomes, it could become another factor for doctors to consider when they are recommending treatment options based on risk. The next step would be to test interventions in clinical trials. “We could make programs targeted toward patients with higher risk, whether it be through more aggressive treatment or more aggressive follow-up, that eventually could improve the survival of these patients,” he explained.
In the future, he hopes to explore disparities in outcomes for other solid tumors, including neuroblastoma, Wilm’s tumor, or other soft tissue sarcomas, related to factors such as zip code, neighborhood deprivation index and other indicators of socioeconomic status. “There is also always the biology of different tumors that has an effect on outcomes, but there are systemic things that we can change to help kids do better. That is really interesting to me,” he said. “It’d be nice to see how that plays a factor and if programs targeted towards evening those things out would be of some use in increasing survival.”
Investing in disparities research
But curiosity alone isn’t enough to propel disparities research. It takes resources, too. “Philanthropy is very important,” he said. “Philanthropy creates opportunities for researchers to do the work that they need to do to make a difference.”
The support from CCRF is especially meaningful because it is Onwuka’s first grant as an independent researcher. “I am really grateful for the grant,” he said. “It has helped to kind of kick-start my career, and hopefully the effect of that would be that I could continue to do research that could affect patient care.”
Onwuka hopes that research on pediatric cancer disparities continues to grow. “The more and more opportunities that we create to support funding around this work, the more people who can be drawn to the field and can do the important work,” he said.
Your donation funds researchers like Onwuka.
Your support propels bold ideas forward and empowers researchers to discover treatments that are better and safer for kids, and ensure every child can have a long, healthy life after cancer.