While most kids with leukemia now survive thanks to advancements in pediatric cancer research, an effective cure has remained elusive for MLL-rearranged leukemia. Infants with this especially aggressive blood cancer — which develops when altered forms of the mixed leukemia lineage (MLL) protein fuse to other proteins — face a 5-year survival rate of only 35%.
With support from an Accelerating Impact for Hard-to-Treat Cancer Award from Children’s Cancer Research Fund (CCRF), University of Virginia researcher John Bushweller is pursuing an innovative new way to treat this devastating disease. Bushweller has found that blocking the MLL protein from binding to DNA stops leukemia cell growth completely — like corking a bottle so that nothing can spill out. Now he and his team at UVA Cancer Center are developing drugs to disrupt the DNA binding process.
“Since this is a new way of attacking the leukemia cells, it has the potential to be more effective than existing therapies as well as less toxic,” he explained. “In addition, since this is a very different approach from existing drugs, it is likely that combinations of this new agent with existing drugs will provide unique benefits.”
Childhood leukemia first captured Bushweller’s interest early in his research career. But his motivation to find better cures only grew as he saw children of friends and neighbors develop leukemia — a poignant reminder of all that’s at stake in the lab. “That’s always in the back of my mind,” he said.
The importance of basic research
Bushweller’s lab focuses on transcription factors, which are proteins that affect gene expression by binding to DNA. About a decade ago, he made an important discovery: a specific part of the MLL protein is key to its ability to bind to DNA. “If we disrupt this interaction, it kills off the ability to drive the disease,” he said. “We decided it was worth trying to make a drug that could do the same thing, and that’s what this project centers on.”
But to get to this point took years of patient trial and error in the lab to better understand the role of the MLL protein. When MLL fuses with other proteins, it creates what’s called a fusion protein that combines part of MLL with part of the other proteins. It’s the abnormal fusion proteins that cause the toughest-to-treat cases of leukemia.
“We’ve been looking at all parts of that protein to see which ones are important and how are they helping to drive the disease, and now I think we have a pretty detailed understanding of what different parts of the protein are doing, and that’s what allows us to start trying to do something translational,” Bushweller explained. “Those early steps, which aren’t going to produce a drug immediately, give us the understanding for how to make a drug that could be efficacious, rather just charging in and trying something. If you haven’t done that foundational work, you don’t know what’s important and you can really go down a rabbit hole.”
Investing in new treatments
With that foundational work in place, Bushweller’s team can now focus on making a first-of-its-kind novel drug that would inhibit the MLL protein and developing the right drug potency to be effective. If all goes well, a new drug could be ready for clinical testing in five years. A different class of MLL inhibitor is already in clinical trials, he noted.
“That could have an impact, but I think what we’ve learned with cancer is that you need more than one agent to succeed,” he said. “Cancer will figure out a way around any one particular target, so we need to hit it in different ways, and what we’re proposing is quite different from what’s entered into clinical trials. Secondly, it’s a novel class of target that hasn’t really been probed before and could have utility both therapeutically but also as a tool to study some of the biology.”
This research could eventually help patients with other cancers that involve the MLL protein, including glioblastoma, gastrointestinal, and head and neck cancers. And that’s just one of the reasons why Bushweller is hopeful for the future of even the most aggressive childhood cancers.
“Over the last couple decades that I’ve been at this, our understanding of these proteins that are drivers in many pediatric cancers has increased dramatically,” he said. “I think we have clever ways to try to target them now, so I’m cautiously optimistic on many pediatric cancer fronts. The unique thing about pediatric cancers is they have low mutation rates so usually there’s just one driver. And if you can turn that off, it’s highly likely that you’re going to get a robust therapeutic benefit.”
The potential benefit for patients is huge, but it requires philanthropic investment to push the research forward and get enough data to secure federal funding for larger studies needed to bring a drug to the marketplace. “These kind of foundation grants serve a really critical purpose to help get to that next level,” Bushweller said.
Your donation funds researchers like Bushweller.
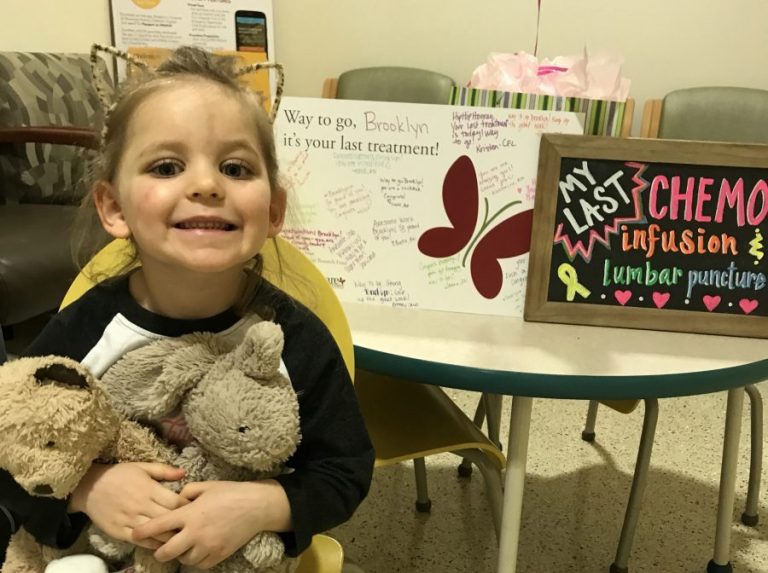
Your support propels bold ideas forward and empowers researchers to discover treatments that are better and safer for kids, and ensure every child can have a long, healthy life after cancer.