Growing up as the child of immigrants, Jenny Ruiz, MD, regularly went to the doctor’s office with her grandfather, a kidney transplant patient who spoke limited English. “Because of our socioeconomic and cultural background, he depended on his grandchildren to take him to his appointments and who often ended up interpreting for him,” she recalled. “So that was my introduction to medicine when I was 16 or 17. I saw a lot of things that needed to be improved, and I felt that I could take a role in making those improvements for future patients.”
A few years later, she helped her aunt and uncle, who also had limited English proficiency, after their 1-year-old daughter was diagnosed with leukemia. “I noticed how communication and language really play a role in trying to understand a cancer diagnosis: knowing when to ask questions, what type of questions, when to call the clinic, and just navigating the whole health care system — not knowing the language makes things more complicated,” she said.
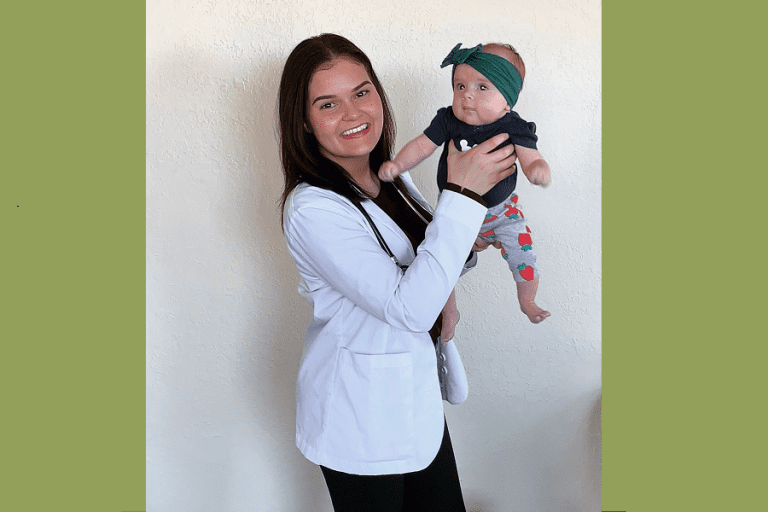
Thankfully, her young cousin was cured — and those experiences inspired Ruiz to pursue a career in pediatric oncology. Now a health equity researcher with Children’s Hospital of Philadelphia, Ruiz is using a grant from Children’s Cancer Research Fund (CCRF) to explore how to make clinical trials more inclusive and equitable. Ruiz is one of the inaugural recipients of CCRF’s new Disparities Award.
“Clinical trials have dramatically improved outcomes in children with cancer over the past 50 years,” Ruiz noted. “However, some racial and ethnic minorities are not fully represented in clinical trials. Children with cancer from historically marginalized racial and ethnic backgrounds experience more side effects and higher relapse rates than the general population. If a clinical trial does not fully represent all people, understanding an individual’s risks for side effects and even how well the treatments work is not possible.”
Understanding the barriers
Ruiz is looking at the potential barriers that can keep patients from historically marginalized backgrounds from enrolling in Phase 1 clinical trials. “These are experimental clinical trials that are the first to get the very basic data of whether or not something is safe in children,” she said. In other words, these are a child’s first chance at a potentially game-changing new treatment — when the clock could be ticking.
Many reasons can prevent a family from enrolling in a clinical trial, from transportation challenges to distrust of the medical system. But sometimes a patient’s family wants to enroll but is not eligible. That’s because patients must meet certain criteria, including a blood count called absolute neutrophil count, or ANC.
“This is a type of white blood cell that helps fight infection as part of your normal immune system,” Ruiz explained. “So the fear is that if you have a low absolute neutrophil count, you’re at higher risk for infections. And also, we don’t want your ANC to be too low before giving you the next cycle of chemotherapy.”
The Children’s Oncology Group requires patients to have an ANC threshold of 1,000, but some industry-sponsored studies require an ANC level of 1,500. “This can potentially be problematic because we know that in the general population, African American individuals have a baseline lower ANC compared to the standardized established norms that were based on a Caucasian population,” Ruiz noted.
A genetic difference common in those with African ancestry can cause lower ANC levels. But Ruiz wants to find out: How much do ANC levels matter? Do patients with an ANC level of 1,000 have more infections or delays to treatment compared to patients who start with a count of 1,500 or 2,000? If there’s not a meaningful difference in outcomes, it could make the case for lowering the enrollment threshold for Phase 1 clinical trials.
“That would mean opening up more trials for more patients,” she said.
Promoting equitable access to care
While this project is focused on ANC levels, Ruiz hopes to explore other potential barriers to clinical trial enrollment. “We know that a lot of rural areas have fewer trials. So how can we get into the community? How can we partner with community organizations to bring these trials to that area as opposed to asking someone to travel two or three or four hours to get on a trial?” she said.
Drawing on her own family’s experiences, Ruiz is also interested in studying language accessibility and whether patients/caregivers who speak languages other than English have the ability to enroll in clinical trials.
“My hope is to really promote equitable access to care for pediatric oncology for all patients, knowing that there are some populations that have been marginalized and have had more difficult times dealing with the health care system,” she said.
But it takes financial investment to advance health equity research — a relatively new and growing area of pediatric cancer research.
“Philanthropy is huge, especially for someone who is transitioning into their first faculty job,” Ruiz said. “It’s so important to have the support and the funding from these types of grants to keep our time protected for research and really be able to push forward our research.”
Your donation funds scientists like Ruiz.
Your support propels bold ideas forward and empowers researchers to discover treatments that are better and safer for kids, and ensure every child can have a long, healthy life after cancer.